Coronary Surgery
Adult congenital cardiac surgery refers to the surgical procedures performed on individuals who were born with congenital heart defects but have survived into adulthood. With advancements in medical care, more children with congenital heart diseases are living longer and reaching adulthood, creating a growing need for specialized surgical interventions tailored to their unique needs.
Pathology:
- Atrial Septal Defect (ASD): ASD is a congenital heart defect characterized by a hole in the septum, the wall that separates the two upper chambers (atria) of the heart. This abnormality allows oxygenated blood from the left atrium to mix with deoxygenated blood in the right atrium. ASDs can vary in size and location. Small defects may not cause significant symptoms, while larger defects can lead to increased blood flow to the lungs, potentially causing symptoms like fatigue, shortness of breath, and recurrent respiratory infections.
- Ventricular Septal Defect (VSD): VSD is a defect in the septum that separates the two lower chambers (ventricles) of the heart. It results in an abnormal communication between the left and right ventricles. VSDs can vary in size and location. Small VSDs may close on their own or cause mild symptoms. However, larger VSDs allow oxygenated and deoxygenated blood to mix, leading to increased blood flow to the lungs. Symptoms can include poor weight gain, difficulty feeding, rapid breathing, and frequent respiratory infections.
- Tetralogy of Fallot (TOF): TOF is a complex congenital heart defect characterized by four abnormalities: a ventricular septal defect (VSD), obstruction of the pulmonary outflow tract, an overriding aorta (which straddles both ventricles), and right ventricular hypertrophy (enlargement of the right ventricle). These abnormalities result in reduced blood flow to the lungs and mixing of oxygenated and deoxygenated blood. Infants with TOF may have cyanosis (blue-tinted skin), poor weight gain, episodes of fainting, and difficulty breathing, particularly during exertion.
- Coarctation of the Aorta (CoA): CoA is a narrowing of the aorta, the major artery that carries oxygenated blood from the heart to the body. The narrowing can occur in different locations along the aorta. CoA can lead to increased blood pressure in the upper body and reduced blood flow to the lower body. Infants with severe CoA may have weak pulses or low blood pressure in the lower body, while older children and adults may experience high blood pressure, headaches, cold legs or feet, and exercise intolerance.
- Transposition of the Great Arteries (TGA): TGA is a condition where the two main arteries, the pulmonary artery and the aorta, are switched in position, causing the oxygenated and deoxygenated blood to circulate independently. This results in inadequate oxygen supply to the body. Newborns with TGA may have cyanosis shortly after birth. Other associated defects, such as ASD or VSD, may be present to allow some mixing of blood, temporarily improving oxygenation.
- Ebstein Anomaly: Ebstein anomaly is a rare congenital heart defect in which the tricuspid valve, which separates the right atrium and right ventricle, is abnormally formed. The valve is displaced downward into the right ventricle, causing leakage of blood back into the atrium. The right ventricle may be small and poorly functioning, and the atrium may be enlarged. Symptoms can range from mild to severe and may include cyanosis, heart palpitations, fatigue, and shortness of breath.
Understanding the specific pathology of each congenital heart defect helps guide the appropriate surgical interventions and post-operative care required for optimal management and long-term outcomes.
Types of Surgery:
Repair of structural abnormalities: This type of surgery aims to correct anatomical defects such as septal defects (holes in the heart), valve abnormalities, or abnormal connections between blood vessels.
Palliative procedures: Some complex congenital heart defects may require staged surgeries to improve the overall circulation or relieve symptoms. These procedures may be performed to redirect blood flow or create temporary pathways to improve oxygenation.
Valve replacement or repair: If the heart valves are defective or damaged, surgical intervention may be necessary to repair or replace them. Valve repairs aim to preserve the native valve tissue, while valve replacements involve implanting mechanical or biological prosthetic valves.
Heart transplantation: In severe cases where the heart is extensively damaged or if previous surgeries have failed, heart transplantation may be the only viable option. This involves replacing the patient’s diseased heart with a healthy donor heart.
Pre-Surgical Care:
Before surgery, a thorough evaluation is conducted to assess the patient’s overall health and the severity of the congenital heart defect. This includes a comprehensive medical history, physical examination, imaging studies (such as echocardiography and cardiac catheterization), and various diagnostic tests. The patient’s condition is optimized through medication management, lifestyle modifications, and, if necessary, preoperative interventions to stabilize the heart and improve outcomes.
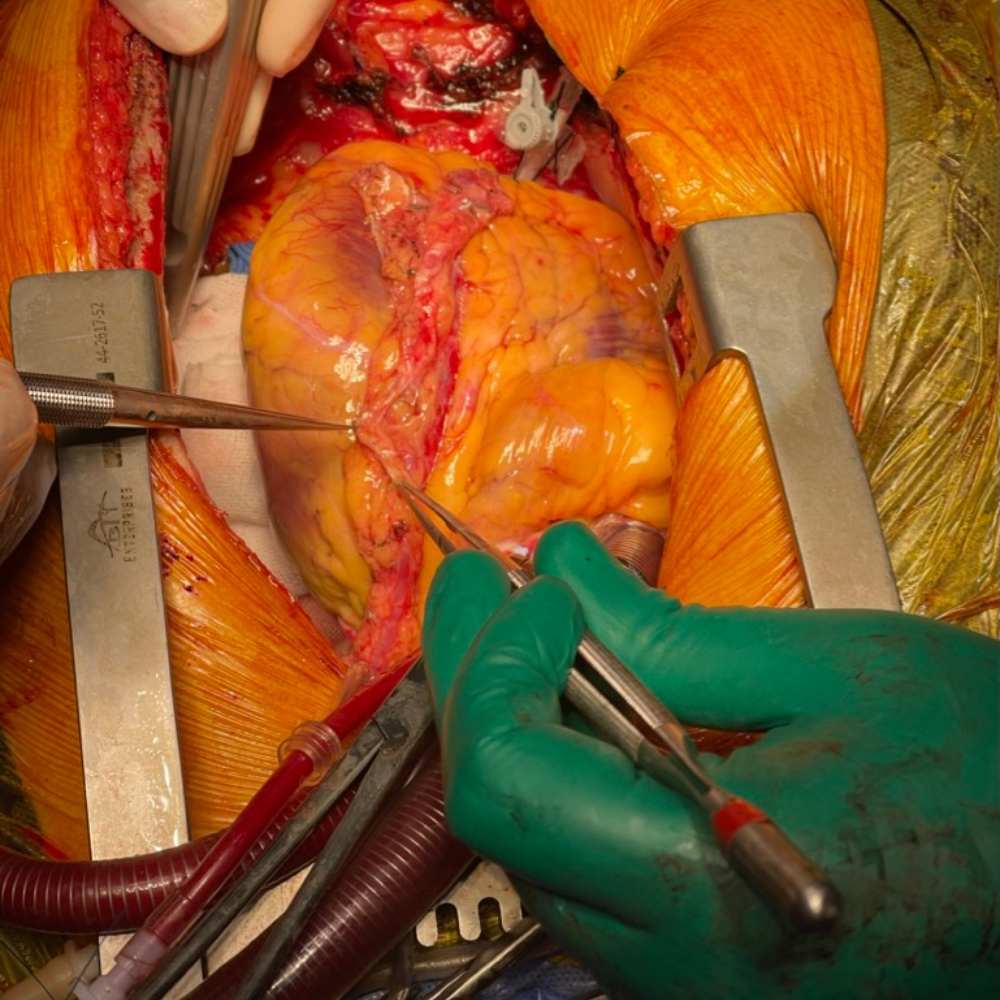
The Surgical Procedure:
The specific surgical procedure depends on the type and severity of the congenital heart defect. It typically involves open-heart surgery, which requires the use of a heart-lung bypass machine to temporarily take over the heart’s pumping function. The surgeon makes an incision in the chest, accesses the heart, repairs or reconstructs the abnormal structures, and ensures proper circulation and oxygenation. The surgery may involve patching holes, widening narrowed blood vessels, reshaping valves, or repositioning arteries and veins. Minimally invasive techniques may also be used when appropriate.
Post-Surgical Care:
After surgery, the patient is closely monitored in the intensive care unit (ICU) to ensure stable vital signs, adequate pain management, and early detection of any complications. The duration of the ICU stay varies depending on the complexity of the surgery and the patient’s overall condition. Post-operative care includes close monitoring of cardiac function, administration of medications, wound care, physical rehabilitation, and patient education regarding lifestyle modifications and ongoing management of the congenital heart condition.
Long-term Follow-up:
Adults who undergo congenital cardiac surgery require lifelong follow-up care. Regular check-ups, imaging studies, and functional assessments are conducted to monitor cardiac function, detect any recurring or new abnormalities, and address potential complications. Medication management, cardiac rehabilitation, and lifestyle modifications are essential components of long-term care to ensure the best possible outcomes and improve the patient’s quality of life.
In summary, adult congenital cardiac surgery is a specialized field that addresses the unique needs of individuals born with congenital heart defects who have reached adulthood. Advances in surgical techniques and comprehensive pre- and post-operative care have significantly improved outcomes for these patients, allowing them to lead fulfilling lives with better heart function and reduced symptoms.
Online Booking

I have performed over a 60 AVNeo cases by myself since 2019. My patients appreciate having an aortic valve using their own tissue, and they are happy to know that the valve is very well working & Doing their physical activity as before. We do all ages including pediatrics and adults.
Prof.Mohammed Sanad , Faculty of Medicine,Mansoura University